Published on: May 29, 2025
If you’re constantly clearing your throat, battling stubborn bad breath, or feel like something’s stuck in the back of your mouth: post-nasal drip might be to blame. And if you’ve recently noticed small white or yellow lumps on your tonsils, there’s a good chance that this drip is doing more than just annoying you. It could be leading to tonsil stones.
In this article, you’ll learn:
- How post-nasal drip creates the perfect conditions for tonsil stones
- Why mucus buildup matters more than you think
- What common signs link the two problems together
Understanding the cause is the first step to breaking the cycle, and knowing what to look for can help you prevent things from getting worse.

How are post-nasal drip and tonsil stones related?
Post-nasal drip creates the perfect storm for tonsil stones to form. When your body makes too much mucus, it can slide down the back of your throat and coats your tonsils.
This sticky mucus traps food bits, bacteria, and dead cells from your mouth and throat. All that gunk settles into small pockets in your tonsils called tonsil crypts. If it’s not cleaned out, it hardens over time and turns into tonsil stones (also called tonsilloliths) [1].
Here’s a quick step-by-step breakdown of how this process unfolds:
- Excess mucus from post-nasal drip slides down the back of your throat.
- That mucus traps food particles, bacteria, and dead cells.
- The sticky buildup gets caught in your tonsil crypts (those little pockets in your tonsils).
- Over time, the trapped debris calcifies, forming small, hard tonsil stones.
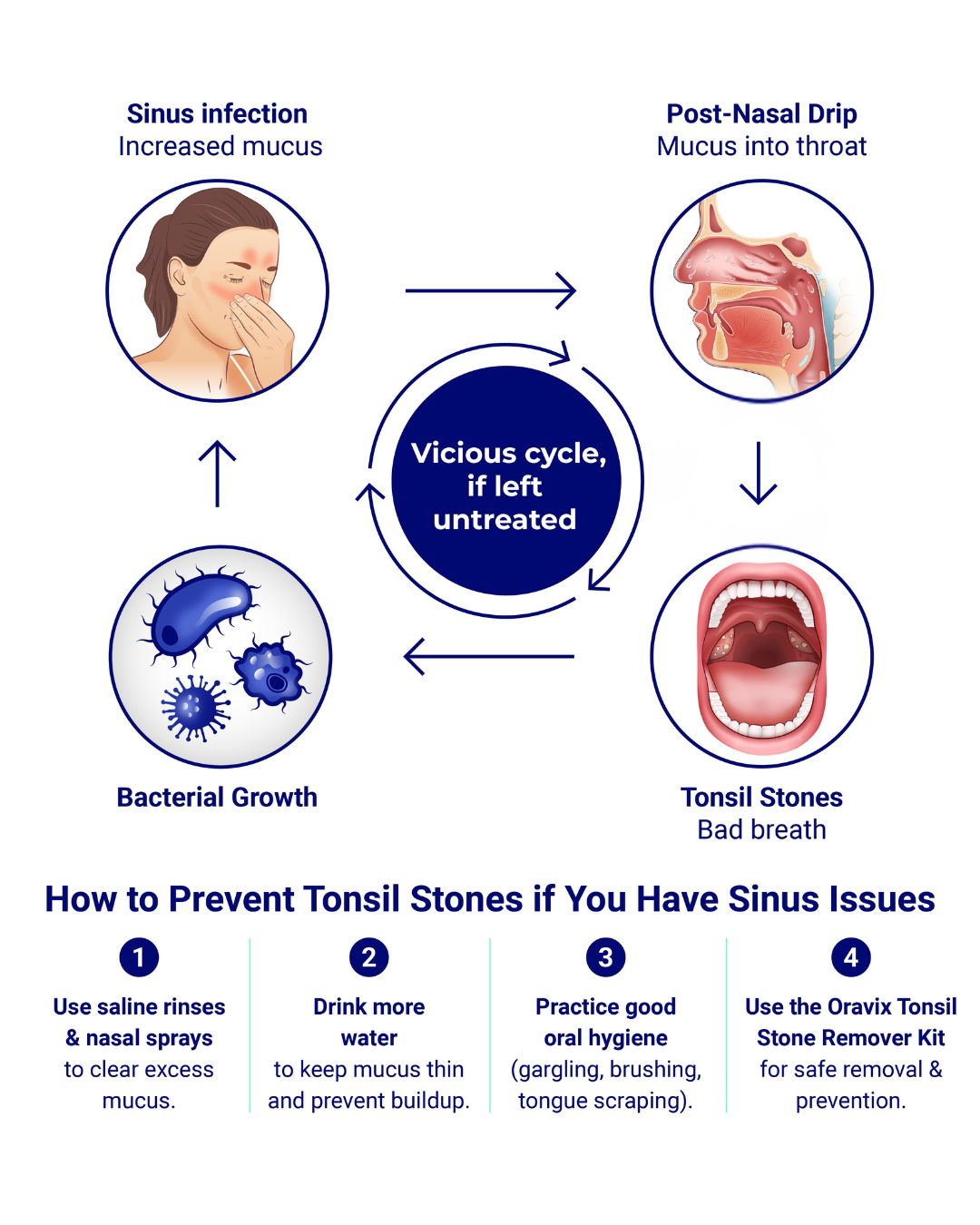
This whole process can lead to other issues, such as:
- Bad breath (halitosis): Tonsil stones contain sulfur-producing bacteria. As the debris breaks down, it releases volatile sulfur compounds—the main cause of persistent bad breath.
- Chronic throat irritation: Mucus buildup and hardened stones can scratch or inflame the tonsils, causing soreness or the constant feeling that something is stuck in your throat.
- Frequent throat clearing and coughing: As mucus lingers and stones form, your body tries to clear the throat, leading to a dry cough or the urge to swallow frequently.
Clinicians note that even when post-nasal drip isn’t painful, it often signals an underlying issue like reflux or allergies, which silently raise your risk of tonsil stones forming [2].
Can Mucus Turn Into Tonsil Stones?
Mucus doesn’t turn into stones on its own. But it acts like glue, trapping bacteria, dead cells, and leftover food particles in your throat, especially after eating or during post-nasal drip. When this mix of debris gets stuck in the deep pockets of your tonsils (called crypts), it can harden over time and form tonsil stones if it’s not removed by swallowing, saliva, or good oral hygiene.
Certain conditions can speed up this process:
- High dairy or sugar intake: stimulates excess mucus production
- Sinus infections or allergies: increase mucus flow and inflammation
- Not drinking enough water: reduces saliva, which normally helps flush away debris
- Smoking: dries out the throat, thickens mucus, and irritates tonsil tissue
In short, mucus acts as the delivery system, and your habits and health determine how much buildup collects in your tonsils.
Can Allergies Give You Tonsil Stones?
Yes, allergies can lead to tonsil stones. Allergies are one of the most common causes of chronic post-nasal drip, which makes them a hidden reason for tonsil stones.
Here’s how it works:
When you breathe in things like pollen, dust, or pet dander, your immune system sees them as threats. To protect you, your body produces extra mucus to trap and get rid of them. But this thick mucus can build up in your throat instead of clearing out, and the perfect conditions to create tonsil stones are created, as we saw earlier.
Over time, this constant drip can also irritate your tonsils and lead to deeper crypts, making it easier for debris to collect and harden into stones.
Some allergy medicines like antihistamines can help reduce the mucus, but they also dry out your mouth. When your mouth is dry, there’s less saliva to clean away the bacteria and gunk, which can make your bad breath even worse. It’s preferable to use non-drying antihistamines (like loratadine or cetirizine) to manage allergies with less risk of dry mouth.
If your tonsil stones show up more during allergy season, it’s likely the two are connected. Treating your allergies may help reduce mucus and your risk of tonsil stones.
Final Thoughts: Why Post-Nasal Drip Can Lead to Tonsil Stones
When excess mucus from post-nasal drip coats your tonsils, it creates a sticky trap for bacteria, dead cells, and food particles. Over time, this debris accumulates and hardens – forming tonsil stones.
Key takeaways:
- Post-nasal drip is a major cause of tonsil stones, especially if it’s chronic or caused by allergies or reflux.
- Mucus acts like glue, trapping debris that calcifies in your tonsils.
- Allergies, diet, dehydration, and smoking all increase your risk by either thickening mucus or drying out your mouth.
If you’ve noticed your symptoms are worse during allergy season or after a cold, this may be the reason.
And if you want to stop stones before they start, don’t miss:
👉 5 Ways to Prevent Tonsil Stones from Post-Nasal Drip
FAQ: Does post-nasal drip always cause tonsil stones?
No, post-nasal drip doesn’t always cause tonsil stones, but it raises your risk significantly, especially if the mucus is thick, you’re dehydrated, or you have poor oral hygiene.
This article offers general oral health info and isn’t a substitute for professional advice. Always consult your dentist or healthcare provider with any medical questions.
References
- Ryan M. W. (2010). The patient with “postnasal drip”. The Medical clinics of North America, 94(5), 913–921. https://doi.org/10.1016/j.mcna.2010.05.009
- Smallwood, D., Ledford, D., Kennedy, D., & Lockey, R. (2024). Postnasal Drip. The journal of allergy and clinical immunology. In practice, 12(6), 1472–1478. https://doi.org/10.1016/j.jaip.2024.04.030

I’m a biomedical engineer turned content writer with over a decade of experience in the healthcare industry and a Master’s Degree in Biological Sciences. I’m passionate about transforming complex scientific research into accessible content to help readers make informed decisions about their health.